This site is intended for U.S. Healthcare Professionals.
Brought to you by Bristol Myers Squibb and Pfizer
Visit Patient Site
AFib & Stroke Risk
AFib & Stroke Risk
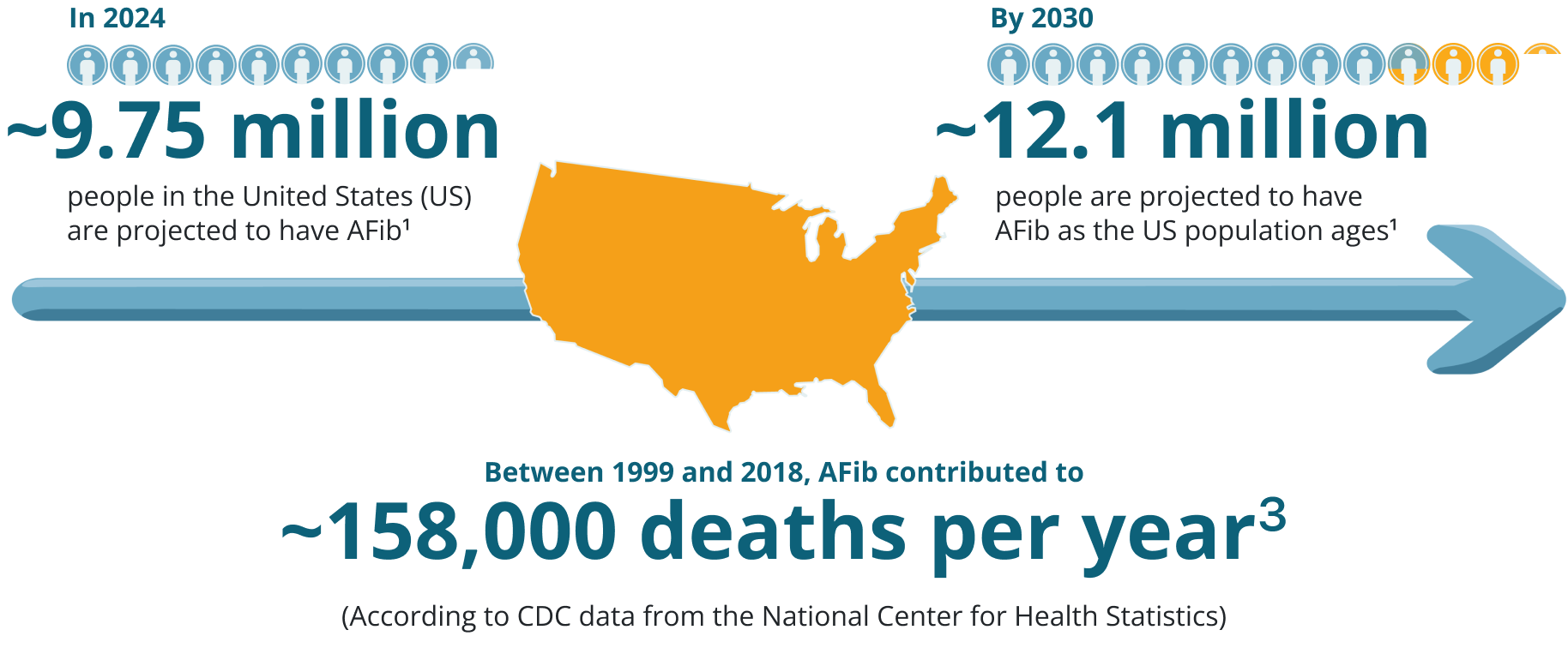
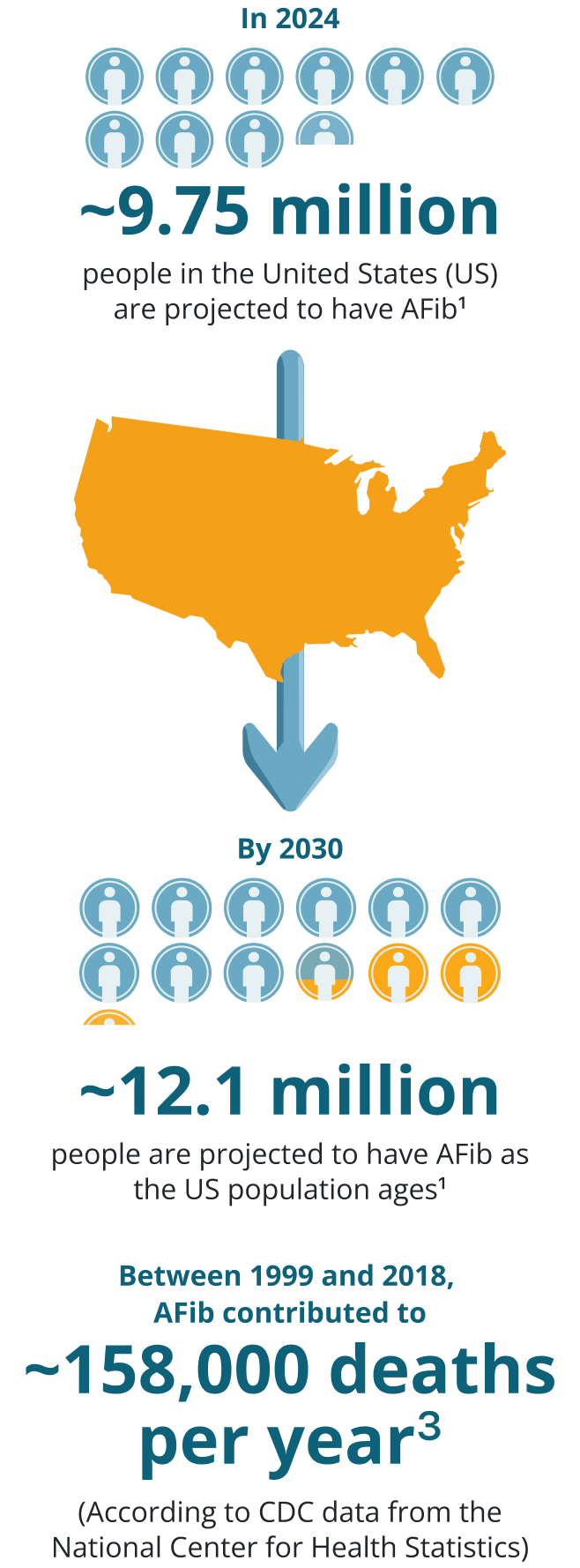
Prevalence and Impact of AFib
Ami Bhatt, MD, FACC, discusses the prevalence of AFib and the associated risk of stroke
AFib is associated with
increased stroke severity4
AFib is associated
with increased
stroke severity4
In the
Framingham Study4:
- Strokes in patients with AFib were associated with increased severity and mortality compared to non-AFib–related strokes*
- The 30-day post-stroke mortality rate, based on an age-adjusted model, demonstrated a 1.84-fold increased risk of death at 30 days post-stroke compared to non-AFib–related strokes
*Among 501 initial ischemic strokes, 103 (20%) had documented AFib.
Study objective: Evaluate the influence of AFib on stroke severity, mortality, and functional disability by means of systematic and serial assessments in stroke subjects using the
Study limitations: Social and psychological factors were not evaluated and not all stroke survivors attended each set-time follow-up examination, which may have introduced bias into the analyses.
AFib may be first discovered
upon admission to the hospital
for a stroke
AFib may be first
discovered upon
admission to the hospital for a strokeIn an additional analysis of
the Framingham Study5:
- During 38 years of follow-up, 656 initial strokes occurred and 115 of these strokes occurred in association with AFib
- 21/115 people had AFib discovered for the first time upon admission for the stroke
- 89/115 had prior documentation of AFib and 5/115 were in sinus rhythm on admission but developed AFib during acute hospitalization for stroke
Study objective: Evaluate and study the relationship between acute stroke and admission-detected AFib in patients suffering stroke without previous diagnosis of atrial fibrillation.5
Study limitations: The number of study cases was small, accuracy of classification of AFib was affected by length and intensity of follow-up, poorer survival rate for AFib subjects during the follow-up period, and without continuous electrocardiogram monitoring, misclassification of the type of AFib could have happened. A portion of the study subjects (6/26) with newly discovered AFib died shortly after stroke onset (within 3 to 25 days), which inherently weakened the ascertainment of the course of AFib.5

AFib is the most common cardiac rhythm disturbance, and AFib-related
strokes are more severe and fatal than strokes not due to AFib.3,4
AFib can present in various ways
While understanding the impact of AFib and related stroke risk is crucial, it is equally important to examine the different presentations and classifications of AFib.
Patients experiencing AFib can be either symptomatic or asymptomatic, which can make diagnosis challenging. Patients with asymptomatic (or silent) AFib do not present with symptoms but do remain at-risk for stroke.6
AFib is characterized by duration of episodes, which often increase in frequency and duration over time. To understand AFib, it’s important to understand the classifications. Classifications of AFib are defined as follows6:
- Paroxysmal: AFib that terminates spontaneously or within 7 days of onset; episodes may occur with variable frequency
- Persistent: Continuous AFib sustained for more than 7 days
- Long-standing: Continuous for more than 12 months
- Permanent: Terminology used when both patient and clinician make a decision to discontinue intervention to maintain or restore sinus rhythm
Examining the presentations of AFib reported in a large-scale national study
Using data from ORBIT-AF, a national observational community-based outpatient registry of 10,087 patients with AFib in the US conducted between June 2010 and August 2011, symptom severity was evaluated at baseline using the physician-assessed EHRA classification system.7
- The EHRA classification system is used to assess and quantify symptoms related to AFib. The EHRA classification is based on the impact of symptoms on daily activity during presumed episodes of AFib
- EHRA proposed scoring system for AFib-related symptoms: 1=asymptomatic, 2=mild, 3=severe, 4=disabling
Within the study, participants fell into 2 categories, asymptomatic and symptomatic based on the EHRA classification.7
Within the study, participants fell into 2 categories, asymptomatic and symptomatic based on the EHRA classification.7
0%
of patients were
asymptomatic
0%
of patients were
symptomatic
- Individual patient-reported symptoms were also assessed, including palpitations, syncope or fainting, dyspnea on exertion, exercise intolerance, lightheadedness or dizziness, dyspnea at rest, fatigue, and chest tightness or discomfort7
- Among patients identified by physicians as asymptomatic using the EHRA score, the vast majority reported no individual symptoms, but 11% reported at least one symptom, with palpitations being the most common (6%)7
EHRA=European Heart Rhythm Association; ORBIT-AF=Outcomes Registry for Better Informed Treatment of Atrial Fibrillation.
Classifications of AFib observed in the ORBIT-AF Study
In the ORBIT-AF study, below are the classifications of AFib, as reported in baseline characteristics of the 10,087 patients, inclusive of both symptomatic and asymptomatic groups.7


(N=1695)
(N=5096)
(N=2819)
(N=477)
Paroxysmal (N=5096)
Persistent (N=1695)
Long-Standing Persistent (N=2819)
New onset (N=477)
Study objective: To assess the symptom severity and quality of life of patients suffering from AFib using the EHRA classification system and AFEQT questionnaire.7
Study limitations: Although the large, community-based cohort included in this study was broadly representative of patients with AFib in the United States, the study evaluated patients who were undergoing treatment for AFib and the results may not be generalizable to a disadvantaged or untreated population.7 The study controlled for a large number of covariates, however a potential limitation of this study may be the presence of residual or unmeasured confounding in the analyses, evaluating the association between AFib symptoms and outcomes.7
AFEQT=AFib Effect on QualiTy of life.

In patients who experience intermittent episodes, or who do not
experience any symptoms, detecting and diagnosing AFib can be
especially challenging.8
It is critical to discuss the signs, symptoms, and risk factors of AFib with patients who are at risk3,9
Your patients may be unaware of the signs, symptoms, and risk factors of AFib.3,9,10
According to a 2019 national survey of 1010 US adults ages 40 and older conducted by The Harris Poll on behalf of the BMS/Pfizer Alliance10:

61%
said that they aren’t familiar with AFib
82%
of non-diagnosed adults wished they knew more about the symptoms of AFib and what to do if they experience them
58%
of adults 65+ did not know that their age can potentially put them at risk for AFib
AFib Signs, Symptoms, and Risk Factors
Ami Bhatt, MD, FACC, shares insights into patient understanding of signs, symptoms, and risk factors for AFib
Help your patients understand AFib signs, symptoms, and risk factors
Some patients are asymptomatic, so it’s important to be mindful of AFib risk factors.6
Risk factors for AFib may include3:
- Advancing age
- Hypertension
- Obesity
- Diabetes
- Heart failure
- Ischemic heart
disease - European ancestry
- Hyperthyroidism
- Chronic kidney disease
- Moderate to heavy alcohol use
- Smoking
- Enlargement of left chambers
of the heart
Signs and symptoms of AFib may include3,9:
- Irregular heartbeat
- Heart palpitations
- Chest pain
- Lightheadedness
- Shortness of breath
- Fatigue

Stay AFib vigilant. Engage your at-risk patients in their care by
discussing the signs, symptoms, and risk factors for AFib